What is Minimally Invasive Spine Surgery?
In order to define Minimally Invasive Spine Surgery, we will need to discuss basic and aging spine anatomy, reasons to have spine surgery (indications) and traditional open spine surgery.
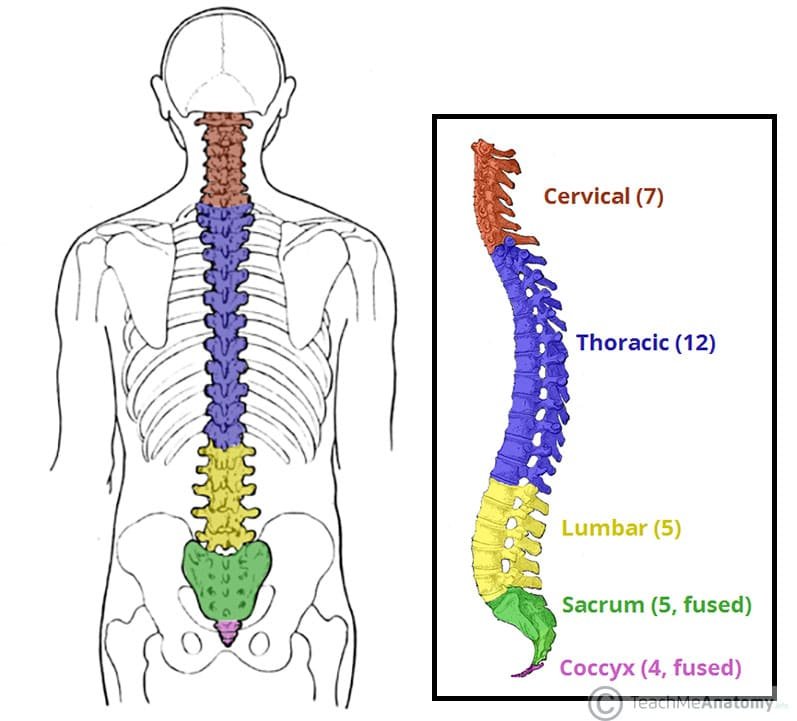
Basic Spine Anatomy
Spine surgery is surgery on the spinal column. The spinal column consists of 33 vertebrae that comprise the human spine and connect the skull to the pelvis. Typically, there are seven cervical vertebrae in the neck, twelve thoracic vertebrae in the midback and five lumbar vertebrae in the lower back as well as five sacral and 4 coccygeal vertebrae, which fuse during development to form the tailbone.
The purpose of the spine is to protect the spinal cord and spinal nerves, which connect the brain to the rest of the body and provide signals for movement, sensation, and other important bodily functions. The spine also provides stability to the body and facilitates motion. Between each vertebrae is a disc in the front of the spine that provides cushion between bones. In the back of each vertebrae are facet joints lined with the same smooth cartilage found in the hip or knee joints, which allow for a gliding motion and provide the spine with flexibility.
The Aging Spine
As we age the discs in the front of the spine degenerate or wear out. Initially discs lose their cushioning material and begin to sag, resembling a flat tire. As the disc space collapses patients lose height. It is not common for a patient with degenerative disc disease to not that they have lost two or more inches of height since they were in their 20s. Patients also begin to tilt forward so that their head is in front of their pelvis in a pitched forward position. Pitched forward posture as a result of spinal degeneration can cause significant pain and disability as the body is forced to compensate through the pelvis, hips and knees to stand upright. These patients often complain of severe lower back pain and inability to stand upright for any significant duration.
As the disc space collapses, there is less cushioning between vertebral bodies which can cause bone on bone contact resulting in bone bruising and back pain. The nerve tunnels on each side of the spine also become collapsed and can cause shooting pain down the arms or legs and even weakness. When the pain shoots down the legs it is called sciatica. Laxity or looseness in the disc space allow excessive motion of the facet joints which can sometimes cause the vertebral bodies to slip forward, a condition known as spondylolisthesis or slipped disc. Disc degeneration tends to run in families and is also related to activity level throughout a patient’s life.
Reasons to Perform Spine Surgery
Generally speaking there are three major reasons to perform surgery on the spine:
Decompression of compressed spinal cord or nerves
Stabilization of unstable vertebral segments
Correction of spinal deformity causing significant disability.
Certain symptoms caused by compression of nerves and spinal cord can be treated with a decompression or clean out surgery in which disc material or bone spurs are removed with microsurgical instruments. Other types of compression caused by unstable vertebral segments and spinal deformities are corrected with stabilization surgery called spinal fusion. This often involves screws, rods and intervertebral cages.
Traditional, Open Spine Surgery
Traditionally, spine surgery was performed through an all-posterior approach with a midline incision and dissection of the paraspinal muscles. These important stabilizing muscles, including the multifidus, were detached from their insertion points on the spine, exposing the bony posterior elements of the spine. Decompression of pinched nerves was achieved by removal of the lamina (Laminectomy).
Unstable segments were treated with spinal fusion. Fusion means turning two objects into one. In the case of spinal fusion this means turning two adjacent vertebrae into one continuous piece or mass of bone. Bone in the back of the spine including the facet joints and transverse processes were ground up with high-speed burrs and packed with bone graft. This tricks the body into thinking that there is a large fracture in the back of the spine and the body heals the fracture by forming a bridge of bone between segments. This bridge connects the bone in the posterolateral aspect of the spine or the posterolateral gutter. This process is called posterolateral spinal fusion or traditional open spinal fusion. Initially this was achieved without the use of screws and rods, a process known as uninstrumented fusion.
Eventually, surgeons discovered that the stability of the spine and rate of fusion success could be enhanced through segmental instrumentation. Initially this was performed with wires and hooks. In the late 1990s, pedicle screws began to receive FDA clearance through 501(k) premarket approval pathways. These screws provided more rigid and stable fixation which led to higher success rates in spinal fusion. Both instrumented and noninstrumented fusions were traditionally performed through a midline incision with extensive dissection of the paraspinal muscles. The muscles are peeled away from their attachments in the middle of the spine and the bones and nerves are out in the open and directly visualized by the surgeon, hence the name traditional open spine surgery.
Deformity correction was performed by careful removal of wedges of bone and compression and distraction of screws to straighten deformities and restore lordosis.
Minimally Invasive Spine Surgery
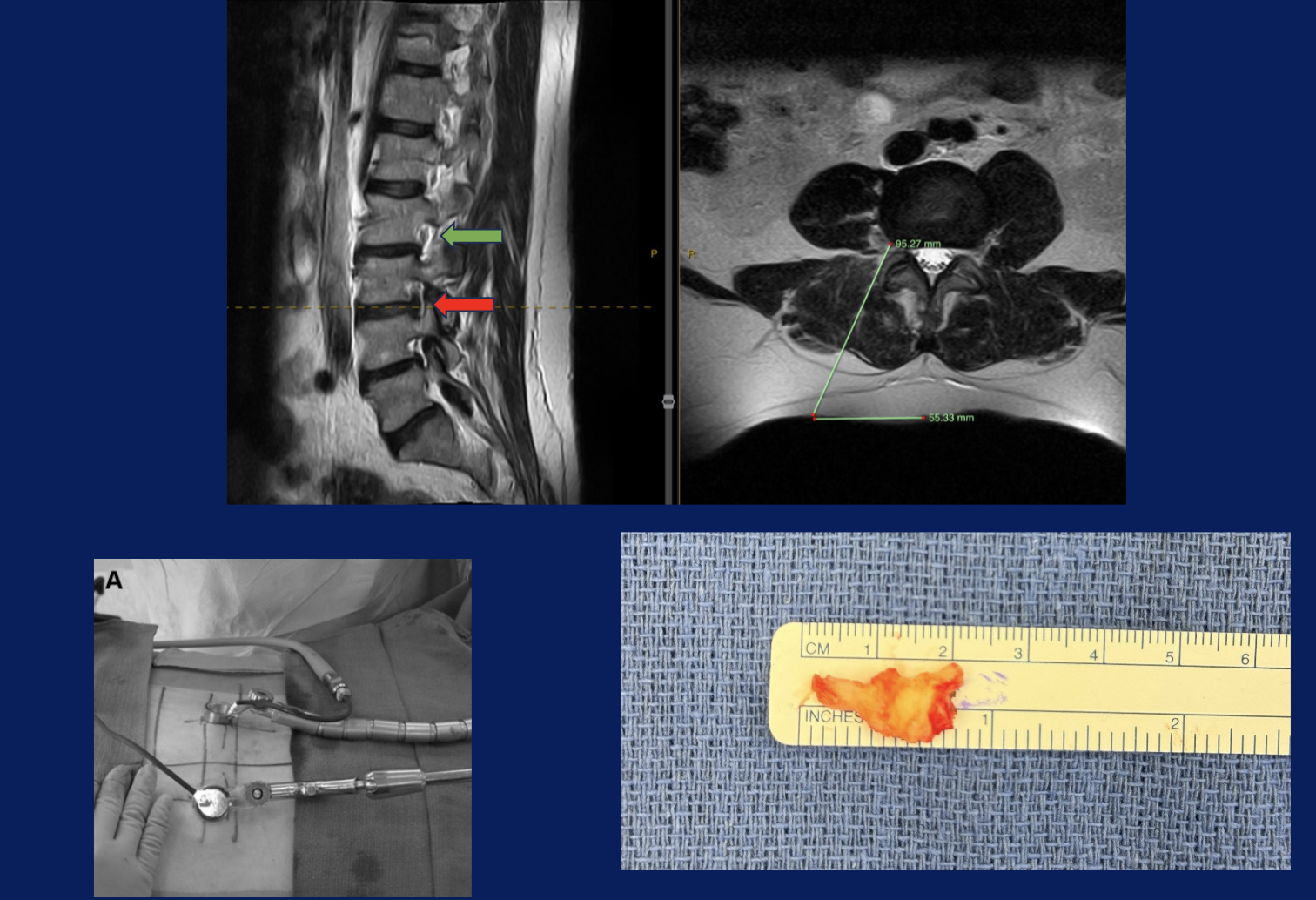
Minimally Invasive Spine Surgery differs from traditional, open spine surgery in that fusion is achieved primarily through the interbody space rather than the posterolateral gutter. This technique is broadly called Interbody fusion. In the lumbar spine this is called Lumbar Interbody Fusion, or “LIF”. Interbody fusion techniques have distinct mechanical and biological advantages over posterolateral fusion, allowing for a large graft with a large surface area to be placed in an area of bony compression which is conducive to healing and fusion. Restoring the height of the disc space leads to improved alignment and also lifts open collapsed nerve tunnels.
Lumbar Interbody Fusion or LIF techniques are named after the direction in which the surgeon approaches the lumbar spine. Anterior Lumbar Interbody Fusion or ALIF involves a direct anterior approach through the patient’s abdomen. Lateral Interbody Fusion LIF, or Lateral Lumbar Interbody Fusion, LLIF, involves approaching though a small incision in the patient’s side between the pelvis and the rib cage. Oblique Lumbar Interbody Fusion (OLIF) involves a similar incision. These anterior techniques allow the surgeon to place a large, stable interbody graft in the front of the spine. Biomechanically this is a very favorable environment for fusion. It is also an excellent way to restore spinal alignment. By distracting the disc space, collapsed nerve tunnels also open up, relieving pressure on pinched nerve roots. This phenomenon is called Indirect Decompression. In traditional open spine surgery, pressure on nerves is relieved through direct removal of lamina (laminectomy), facet joints (facetectomy) and bone spurs in the neuroforamen or nerve tunnel (foraminotomy). These techniques are known as direct decompression. Minimally Invasive Spine Surgery can be performed through a posterior approaches as well Minimally Invasive Surgery Posterior Lumbar Interbody Fusion (MIS PLIF) and Minimally Invasive Surgery Transforaminal Lumbar Interbody Fusion (MIS TLIF).
Minimally Invasive Spine Surgery Techniques are called minimally invasive because they limit damage to the important paraspinal muscles. Paraspinal muscles are a sophisticated network of muscles that provide stability and motion to the trunk. Perhaps the most important of the paraspinal muscles in the multifidus. The multifidus attaches to the spinous processes, which are the bony prominences in the middle of your back. It has bands that attach to the facet joints one two and three levels below. It is a stout muscle with a large physiological cross sectional area. The multifidus becomes stronger when the spine is flexed forward and acts as an important checkrein to excess motion seen in spinal instability. The multifidus is to the human spine as a suspension is to a car.
One major problem with open spine surgery is that it often detaches and injures the multifidus muscle, impairing the natural ability of the spine to stabilize itself. By comparison, minimally invasive techniques involve little to no damage to the paraspinal muscles. When minimally invasive pedicle screws are placed, they are done through an intermuscular plane, or natural division between muscles. Less muscle damage during surgery results in lower blood loss, less postoperative pain and disability, and faster recovery.
Am I a candidate for minimally invasive spine surgery?
This is a question that is highly dependent on the nature of your pathology as well as the experience and comfort level of your surgeon. In general, minimally invasive spine surgery is very helpful in patients with degenerative spinal pathology at one or more levels due to the natural aging of the spine. Minimally invasive spine surgery is especially effective in restoring height and alignment lost due to disc degeneration. Minimally invasive spine surgery is also effective in opening up nerve tunnels that have been closed due to disc collapse.
Minimally invasive spine surgery is also very useful in patients with prior laminectomy (post laminectomy syndrome), pseudarthrosis (failed fusion), or prior operations (failed back syndrome). Often more complex spinal issues can be treated with a hybrid approach, which is a combination of minimally invasive and open techniques.
One of the most fascinating aspects of spine surgery is that there are many ways to address any given problem. Each patient requires a thoughtful and personalized approach taking into account his or her unique history, physical examination, imaging findings, and goals. It is important to have a spine surgeon who is trained in traditional open and minimally invasive techniques in order to determine the best approach for each patient.
Regardless of technique (minimally invasive, traditional open, or hybrid), patients who have surgery that addresses the following concerns tend to experience excellent clinical outcomes:
1)Decompression of compressed spinal cord or nerves
2)Stabilization of unstable vertebral segments
3)Correction of spinal deformity causing significant disability
Why does spinal fusion have a bad reputation to some people?
It is very common for patients to express concern regarding spinal fusion surgery. They may have had a friend or older relative with chronic pain who had a spinal fusion in the past. It is important to remember that there is a wide range of indications and techniques for spinal fusion. Spinal fusion surgeries performed for one of the three goals listed above tend to do very well in terms of experiencing reduced pain and increased function and activity level after spine surgery.
Unfortunately, in the late 1990s and early 2000s there was a great enthusiasm to perform spinal fusion for degenerative disc disease as a cause of axial back pain, or pain in the middle of the back. Many spinal fusions were performed with the goal of treating back pain by fusing spinal motion segments that showed disc degeneration on MRI. The problem with this logic is that MRI and xray findings of disc degeneration and age related wear and tear are extremely common in asymptomatic individuals. In other words, many people with no complaints of back or neck pain will have signs of disc degeneration on their MRI.
When patients undergo a MRI they will often receive a radiologist’s report with detailed descriptions of every finding including degenerative changes related to age appropriate wear and tear. It is important to review your MRI with a qualified spine surgeon who can discuss these findings of concern and also reassure you on findings which are less concerning.
I will frequently tell patients I care a lot more about your symptoms and quality of life than I do about your MRI. MRI findings alone may not be a significant problem. If a focal problem on your MRI correlates with a clinical symptom that you are directly experiencing, then we will consider surgery to address this using minimally invasive techniques when possible. If there is no correlation then we will observe your symptoms over time and I may refer you to a nonsurgical pain management colleague when appropriate.
In spine surgery when the imaging findings correlate with the patient’s history and physical examination and a surgical plan is constructed and executed that addresses these specific goals, there is a very high likelihood of clinical improvement and success. As a patient you should understand what we are doing in a surgery, why we are doing it, risks of the operation, benefits of the operation, and alternatives to surgery.
In my practice we discuss these important matters at the time of surgery scheduling and we review them again in detail during the preoperative visit. When surgical plans do not have specific goals and objectives they are much less likely to be successful. New research is coming out daily to help us select which patients will benefit most from which techniques, but the fundamental principles of spine surgery stand the test of time.
What should I look for in a minimally invasive spine surgeon?
Spine surgeons must complete either orthopedic surgery residency or neurosurgery residency. After residency training, many surgeons choose to pursue an additional specialized training called a fellowship. It is important to find a surgeon who has trained in both traditional open as well as minimally invasive spine surgery so that he or she can choose which techniques are most appropriate. While minimally invasive techniques are taught in spine residency and fellowship programs, many of these techniques are learned and developed in practice as well. Surgeons who are involved in education and teaching of techniques to trainees and peers as well as those who present and publish their work at meetings and in peer reviewed journals are often those who are experienced and able to treat patients successfully with minimally invasive spine surgery.